Leaky Gut Symptoms and Surprising Signs Your Doctor Overlooks
If you’ve ever wondered whether your nagging digestive issues, random skin flare-ups, or stubborn fatigue might be connected, you’re not alone. Many people suspect leaky gut is at the root of their problems, yet struggle to get clear answers—or even acknowledgment—from their healthcare providers. While “leaky gut” is still debated in conventional medicine, there is growing research around increased intestinal permeability and its possible link to a range of symptoms.
This guide breaks down what leaky gut is, the classic and lesser-known symptoms, why your doctor might miss it, and practical steps to support your gut lining.
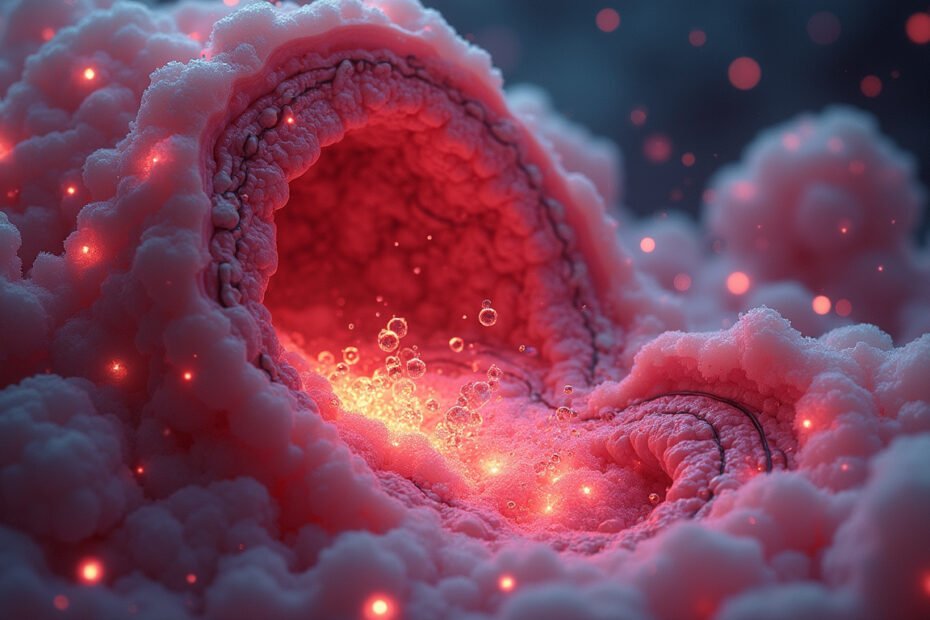
What Is Leaky Gut, Really?
“Leaky gut” is a popular term for increased intestinal permeability. Under healthy conditions, your intestinal lining acts like a tightly woven net:
- It lets in nutrients, water, and electrolytes.
- It keeps out larger particles like undigested food, toxins, and microbes.
This barrier is maintained by structures called tight junctions between intestinal cells. When these junctions loosen, the gut lining becomes more permeable—“leaky.” Larger molecules can pass through into the bloodstream, potentially triggering:
- Immune reactions
- Low-grade inflammation
- Symptoms that show up in organs far from your digestive tract
Researchers are still exploring how increased intestinal permeability may relate to conditions like inflammatory bowel disease, celiac disease, and autoimmune disorders (source: National Institutes of Health).
While not every expert loves the phrase “leaky gut,” increased permeability is real and measurable in research settings.
Classic Leaky Gut Symptoms You Might Recognize
Some symptoms are commonly associated with leaky gut, yet can still be brushed off as “normal” or attributed to stress or aging.
1. Digestive Discomfort and Bloating
Persistent digestive issues are among the most frequently reported signs:
- Bloating after meals
- Excessive gas
- Cramping or abdominal pain
- Constipation, diarrhea, or alternating between the two
- A sense that food “just sits there”
These issues can overlap with IBS, SIBO, or food intolerances, and many people are told they have “functional” gut problems without a clear root cause.
2. Food Sensitivities and Reactivity
When the gut barrier is compromised, partially digested food particles may slip through and interact with the immune system. Over time, your body can start reacting to foods that once felt fine.
Common patterns include:
- Feeling worse after gluten, dairy, soy, eggs, or processed foods
- Headaches, fatigue, or brain fog after certain meals
- Itchy skin or rashes that flare after eating
Food sensitivity testing is controversial and not always accurate, but a noticeable pattern of symptom flare-ups after specific foods may suggest your gut barrier isn’t functioning optimally.
3. Chronic Fatigue and Low Energy
Many people with possible leaky gut report:
- Waking up tired even after a full night’s sleep
- Afternoon crashes
- Feeling wired-but-tired at night
Ongoing immune activation and inflammation can drain your energy reserves, while poor absorption of nutrients (like iron, B12, and magnesium) worsens fatigue.
Surprising Leaky Gut Signs Your Doctor May Overlook
Here’s where things get tricky: some of the most disruptive signs of leaky gut show up outside your digestive system—and that’s exactly why they get overlooked.
4. Brain Fog, Mood Changes, and Poor Focus
The gut and brain communicate through nerves, hormones, and immune signaling—often called the gut-brain axis. When your gut barrier is compromised, inflammatory molecules and immune messengers can influence brain function.
You might notice:
- Difficulty concentrating or feeling “spacey”
- Memory lapses and word-finding issues
- Increased anxiety or irritability
- Dips in mood or mild depressive symptoms
These symptoms are often labeled as stress, burnout, or “just getting older,” even though supporting gut health can sometimes make a surprising difference.
5. Skin Issues: Acne, Eczema, Rashes, and Hives
Your skin is another major interface with your immune system. Research suggests a gut-skin axis, where imbalances in the microbiome or increased intestinal permeability may contribute to:
- Acne or cystic breakouts
- Eczema or atopic dermatitis
- Psoriasis flares
- Recurrent hives or itching without a clear allergy
If topical treatments and steroids give only temporary relief, it may be worth evaluating whether a leaky gut and underlying inflammation are playing a role.
6. Achy Joints and Unexplained Inflammation
Autoimmune and inflammatory conditions are increasingly being studied in relation to gut health and barrier integrity. Symptoms that may be connected include:
- Achy or stiff joints, especially in the morning
- Swelling in hands, wrists, or knees
- Pain that moves around with no clear injury
- High-sensitivity CRP or other inflammation markers on lab tests
While joint pain has many possible causes, there is evidence that increased intestinal permeability may influence autoimmune activity and systemic inflammation.
7. Frequent Illnesses and Weak Immunity
Around 70% of your immune system resides in and around your gut. When the intestinal barrier is compromised:
- The immune system may become overactive in some ways (allergies, autoimmunity).
- It may be underperforming in others (frequent colds, slow recovery).
People with suspected leaky gut sometimes report:
- Getting every cold that goes around
- Slow healing from cuts or minor infections
- Recurring sinus, throat, or respiratory infections
Your doctor might treat each infection as a separate event without looking at how gut health and barrier function fit into the bigger picture.

8. Hormonal Imbalances and Difficult PMS
The gut plays a major role in metabolizing and excreting hormones—especially estrogen. When gut bacteria are imbalanced and the lining is irritated, hormone clearance can be affected.
You may notice:
- Worsening PMS: mood swings, cramps, breast tenderness
- Heavier or more painful periods
- Perimenopausal symptoms that feel more intense than expected
These are rarely linked back to the gut in conventional appointments, but many functional and integrative practitioners consider leaky gut a contributing factor.
Why Leaky Gut Symptoms Are Easy to Dismiss
Even when people show multiple leaky gut symptoms, they often feel dismissed or told “your labs are normal.” There are several reasons for this.
Conventional Medicine vs. Emerging Science
- Terminology mismatch: Doctors are trained to think in terms of “increased intestinal permeability,” not “leaky gut,” which is seen as a vague, alternative label.
- Limited testing: There is no single, widely adopted clinical test for leaky gut, and markers used in research (like zonulin or lactulose-mannitol tests) aren’t standard for most clinics.
- Symptom overlap: Signs like fatigue, bloating, and brain fog overlap with countless other conditions, making it hard to pin them on gut permeability.
Time Constraints and Fragmented Care
- Short appointments make it difficult to piece together skin, mood, digestive, and joint symptoms into one systemic picture.
- Patients often see different specialists—dermatologists for skin, rheumatologists for joints, gastroenterologists for digestion—without anyone asking, “What’s happening in your gut overall?”
Common Triggers and Root Causes of Leaky Gut
Although more research is needed, several factors are repeatedly associated with increased intestinal permeability:
- Highly processed diet: Refined sugar, industrial seed oils, and additives may disrupt the gut lining and microbiome.
- Gluten and certain grains: Especially in people with celiac disease or non-celiac gluten sensitivity, gluten is linked to higher levels of zonulin, a regulator of tight junctions.
- Chronic stress: Stress hormones can alter gut blood flow, motility, and microbial balance.
- Medications: Long-term use of NSAIDs (like ibuprofen), certain antibiotics, and some acid blockers may irritate or thin the gut lining.
- Imbalanced microbiome: Dysbiosis (an overgrowth of harmful microbes and/or loss of beneficial ones) can contribute to inflammation and barrier breakdown.
- Alcohol and smoking: Both can damage the intestinal lining and fuel inflammation.
No single factor causes leaky gut for everyone; it’s usually a combination tipping the balance over time.
How to Support Healing If You Suspect Leaky Gut
If you recognize yourself in these symptoms, you don’t need to wait for perfect tests to start caring for your gut barrier. Always work with a qualified practitioner, especially if you have existing medical conditions, but these strategies are commonly used to support gut health.
1. Focus on a Gut-Supportive Diet
An anti-inflammatory, whole-food approach can reduce stress on your gut lining.
Consider emphasizing:
- Colorful vegetables and low-sugar fruits
- High-quality proteins (fish, poultry, grass-fed meats, legumes if tolerated)
- Healthy fats (olive oil, avocado, nuts, seeds)
- Fermented foods (sauerkraut, kimchi, yogurt, kefir) if you tolerate them
- Bone broth or collagen-rich foods for building blocks of connective tissue
And reducing or eliminating for a trial period:
- Refined sugar and sugary drinks
- Ultra-processed snacks and fast food
- Excess alcohol
- Common triggers like gluten, dairy, or soy (short-term elimination followed by careful reintroduction can be informative)
2. Rebuild the Microbiome, Gently
The right microbiome balance helps maintain the gut barrier:
- Include prebiotics (fibers that feed beneficial bacteria): onions, garlic, leeks, asparagus, green bananas, oats, and beans if tolerated.
- Consider a probiotic supplement or diverse fermented foods. Start low and slow to avoid excessive gas and bloating.
3. Manage Stress and Sleep
Your gut lining regenerates heavily at night, and stress directly affects gut motility and permeability.
Helpful habits include:
- 7–9 hours of sleep with a consistent schedule
- Daily nervous system “breaks”: deep breathing, meditation, gentle yoga, or walking
- Setting boundaries around work and screen time, especially before bed
4. Use Supplements Strategically (Under Guidance)
Commonly suggested gut-supportive nutrients include:
- L-glutamine – a key fuel for intestinal cells
- Zinc – important for tissue repair
- Omega-3 fatty acids – to help calm inflammation
- Vitamin D – crucial for immune regulation
Only start supplements under professional guidance, especially if you take medications or have chronic illnesses.
When to Talk to Your Doctor (and What to Ask)
If you’re concerned about leaky gut symptoms:
-
Document your symptoms
- Track digestion, sleep, energy, mood, skin, and joint pain for 2–4 weeks.
- Note any patterns related to food, stress, or your menstrual cycle (if applicable).
-
Bring specific questions
You might ask:- “Could food sensitivities or intestinal permeability be contributing to my symptoms?”
- “Would it be appropriate to check for celiac disease, nutrient deficiencies, or inflammatory markers?”
- “Is there a referral to a gastroenterologist or integrative practitioner who can look deeper at my gut health?”
-
Advocate for yourself
If your concerns are dismissed, consider a second opinion—especially with a provider familiar with functional or integrative medicine, who may be more open to exploring increased intestinal permeability as part of the puzzle.
FAQ About Leaky Gut and Overlooked Symptoms
Q1: How do I know if I have leaky gut syndrome vs. just IBS?
IBS shares many symptoms with leaky gut, including bloating, cramping, and irregular bowel habits. However, if you also experience issues like skin rashes, brain fog, food sensitivities, or joint pain, it may suggest a more systemic problem potentially linked to intestinal permeability. There’s no universally accepted test for leaky gut syndrome, so clinicians often look at symptom clusters and underlying triggers rather than a single lab result.
Q2: Can leaky gut cause anxiety and mood issues?
Emerging research around the gut-brain axis suggests that changes in the microbiome and gut barrier can influence mood and anxiety through inflammatory pathways, neurotransmitter production, and vagus nerve signaling. While leaky gut is unlikely to be the only cause, supporting gut health—via diet, stress management, and lifestyle—can sometimes reduce anxiety and improve overall mental clarity.
Q3: What are the first steps to heal leaky gut naturally?
The most foundational steps are to reduce inflammatory triggers, repair the gut lining, and rebalance your microbiome. That usually means shifting toward a whole-food, low-processed diet, limiting alcohol and irritants, managing stress, prioritizing sleep, and introducing gut-supportive nutrients and fibers. Working with a practitioner who understands leaky gut and gut dysbiosis is the safest way to tailor these steps to your unique situation.
Listen to Your Body—and Take the Next Step
If your symptoms have been dismissed as “just stress,” “IBS,” or “aging,” yet you feel in your gut that something deeper is going on, it’s worth exploring the possibility of leaky gut. Your digestion, skin, mood, joints, and immune system are all interconnected, and your gut is at the center of that web.
You don’t have to accept bloating, fatigue, or brain fog as your new normal. Start by tracking your symptoms, making small but consistent changes to your diet and lifestyle, and seeking out a practitioner who takes your experience seriously and understands intestinal permeability. The sooner you support your gut barrier, the sooner you may start to see whole-body improvements.
Take the next step today: commit to one gut-supporting change this week—whether it’s cutting back on processed foods, adding a daily walk, or booking an appointment with a gut-focused clinician—and give your body the chance to begin repairing from the inside out.
This post may contain affiliate links which means I may receive a commission for purchases made through links. I will only recommend products that I have personally used! Learn more on my Private Policy page.